Histamine is a biogenic amine that is released from mast cells within the immune system when an allergen is detected by the body. When the body releases histamine, healthy individuals are able to break down the excess histamine with a specific enzyme called diamine oxidase (DAO). Histamine intolerance is a condition that arises when there is an imbalance between excessive histamine ingestion with food or deficient histamine breakdown in the body.
Histamine intolerance displays symptoms, such as rhinitis, headache, gastrointestinal symptoms, skin-swelling, eczema, palpitations, hives, and itching. People with histamine intolerance may also have lower gut diversity or degraded gut flora. The prevalence of histamine intolerance is estimated to be 1-4% of the population.
If your client demonstrates common symptoms associated with histamine intolerance and has tested negative for other allergies or gastrointestinal conditions, you can consider trialing a low histamine diet to relieve symptoms. In this article we will cover:
- Key principles for a low histamine diet.
- Steps for low histamine meal planning.
What is a Low Histamine Diet?
A low histamine diet requires the restriction or elimination of any food, ingredient, or substance that contains high amounts of histamine, which triggers an allergic response. Decreasing consumption of histamine can significantly reduce allergy symptoms, and it may even increase DAO levels in the blood.
After food allergies have been ruled out, a low histamine diet is often recommended, and a favorable response to it can help diagnose histamine intolerance.

Who is a Low Histamine Diet For?
An effective method for reducing the symptoms of histamine intolerance is to carefully follow a histamine-restricted diet, in combination with a DAO supplement.
Every histamine-sensitive individual has a threshold of histamine or histamine-releasing foods they can tolerate before experiencing symptoms. Nutrition professionals can work with clients to implement an individualized low histamine diet and then gradually add foods back to identify how much histamine an individual can tolerate.
Adjusting for each individual’s unique needs is important and often necessary. Following a low histamine diet with guidance from a nutrition professional could optimally nourish a client with histamine intolerance.
Foods to Eat & Avoid
The amount of histamine from dietary sources can vary. Histamine is a by-product of bacterial metabolism so aged and fermented foods like cheeses, yogurt, processed meats, alcoholic beverages, kefir, kombucha, sauerkraut, and soy are typically high in histamine.
Meat and poultry have two pathways of histamine production through microbial-developed histamine and from the denaturation of protein during cooking as the histamine level in food changes according to the cooking method. Special attention needs to be paid to fish as consuming spoiled fish can lead to scombroid poisoning, where the bacteria releases histamine.
Plain, freshly cooked meats are safe to eat. Freezing leftover protein foods such as meat, poultry, and fish is encouraged to slow bacterial growth and histamine production. Since bacteria multiply rapidly, eating leftover animal products that have been stored at room temperature or even in the fridge should be avoided.
There are some foods that appear to naturally have higher levels of histamine which block the DAO enzyme and there are foods that contain amines that are similar to histamine and can compete for DAO:
- Certain food additives, artificial flavorings, artificial colors such as tartrazine, and preservatives such as benzoates and sulfites.
- Certain fruits and vegetables, such as apricots, cherries, citrus fruits, avocado, eggplant, spinach, and pumpkin.
- Legumes like chickpeas, lentils, and kidney beans.
- Spices like chili powder, cinnamon, cloves, and nutmeg.
Most fruits and vegetables are protected by their peels or skins from germs, and therefore histamine production. Encourage your clients to peel and prepare their fruits and vegetables close to eating. Foods that are minimally processed and milk, cream, many grains, plain spices and herbs, and several different fruits and vegetables are safe to eat.
Freshness has an impact on how much histamine a food contains so it is important to teach clients when to shop and cook to keep foods fresh and how to safely store foods to limit histamine levels.
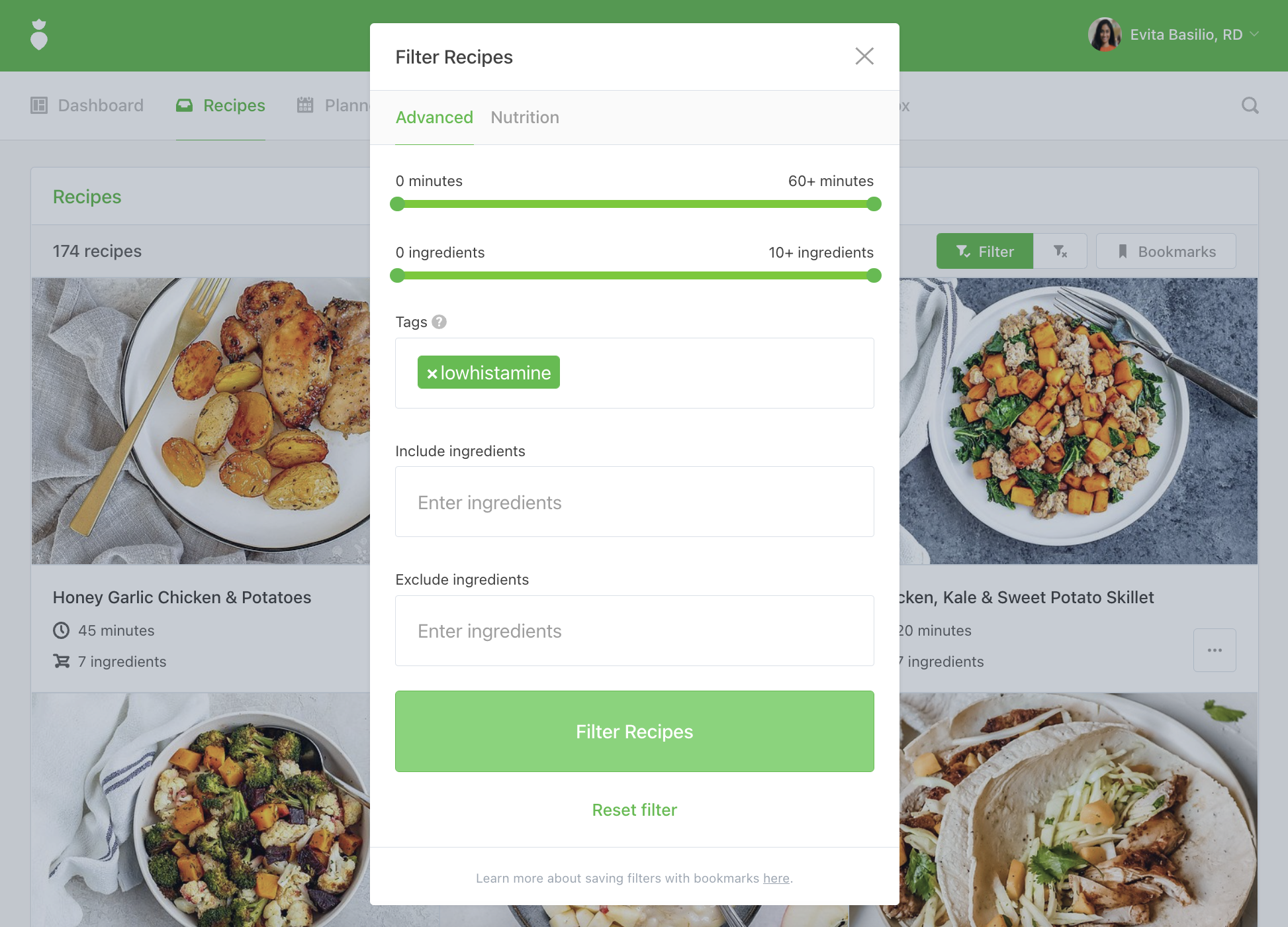
Tip: Log into That Clean Life and use the low histamine filter to find recipes and our Low Histamine Diet for full done-for-you meal plans with grocery lists, recipes, prep guides, and supporting evidence.
Low Histamine Meal Planning Steps
The low histamine diet can be implemented in a phased approach:
1. Avoidance
Histamine-containing foods should be avoided for a period of two to four weeks as a trial to assess whether symptoms improve. The goal of this phase is to reduce symptoms to the greatest possible extent. If a positive response is noted, you may assume that it is a histamine sensitivity and a low histamine diet would be required long-term.
Tip: Here are 20 low histamine meal ideas including breakfasts, lunches, dinners, and snacks that we know your clients will love!
2. Reintroduction
Each individual has a personal limit of histamine tolerance and the elimination phase should be followed by up to six weeks of reintroducing foods slowly to determine histamine tolerance while taking the client’s individual dietary preferences into consideration. Encourage your clients to keep a symptom journal during this phase to record any allergic reaction. This phase will help increase the variety of foods allowed and determine a tolerance threshold that will serve as a basis for planning long-term dietary changes.
3. Maintenance
The final stage is determining what your client’s long-term diet might look like. The nutritional recommendations should be guided by the individual’s histamine tolerance and dietary preferences to create a balanced diet and improve their quality of life.

The best way to minimize the recurrence of histamine intolerance symptoms is to maintain an individualized low histamine diet. As a long-term exclusion diet, it should be closely monitored by a nutrition professional to optimally nourish and assess for potential deficiencies.
It will be beneficial to work with a physician to add a DAO supplement and micronutrient supplements which may increase the effectiveness of DAO enzymes. All medications and supplements should be free of artificial colors and preservatives.
Learn more about That Clean Life's Low Histamine Diet here.

