Nutrition is just one piece to help your clients balance their insulin levels and achieve their glucose targets. But lifestyle factors and self-management skills are also necessary for your clients to be successful.
Supporting your clients when it comes to balancing their blood sugar needs to go beyond a simple meal plan. Here are some straightforward strategies you can include with your nutrition plan to optimize your clients' blood sugar levels.
1. Incorporate Daily Physical Activity
Physical activity improves glucose control, helps with weight management, reduces stress, and lowers blood pressure. On the other hand, sitting for long periods of time is associated with an increased risk of death and major cardiovascular events.
Guidelines recommend breaking up sitting periods while aiming to get at least 150 minutes per week of aerobic exercise and at least two sessions per week of resistance exercise.
Help your clients integrate more physical activity into their lives by:
- Assessing any barriers they might face when it comes to physical activity and developing strategies to overcome them.
- Setting specific activity goals.
- Helping them find activities they would enjoy.
2. Seek Mental Health Support
Changes in blood sugar levels can alter mood and cause symptoms of fatigue, trouble thinking clearly, and anxiety. People living with diabetes are also at increased risk for depression, anxiety, eating disorders, and a condition called diabetes distress which shares some traits of stress, depression, and anxiety.
All individuals with diabetes should be regularly screened for the presence of diabetes distress, as well as symptoms of common psychiatric disorders.
Encourage your clients to spend time tuning into their emotions, and talking to their friends, family, and members of their healthcare team about how they are feeling. Help clients to learn effective coping skills and direct them to support services that can make a difference for their mental health.

3. Get Enough Sleep
Too little or too much sleep and poor sleep quality can impact insulin sensitivity, glucose tolerance, and appetite regulation.
Encourage your clients to get seven to eight hours of undisturbed sleep per night by using strategies such as:
- Avoiding blue light three hours before bed.
- Introducing magnesium and melatonin supplements.
- Using herbal teas and guided meditations.
4. Ensure Proper Hydration
People living with diabetes have an increased risk of dehydration as high blood glucose levels lead to decreased hydration in the body.
The amount of fluid your client needs depends on a variety of factors including age, gender, stress, physical activity, and climate. Provide a personalized hydration target for your client's unique needs and make hydration fun with herbal teas, fruit-infused waters, and fruit-free green juices.
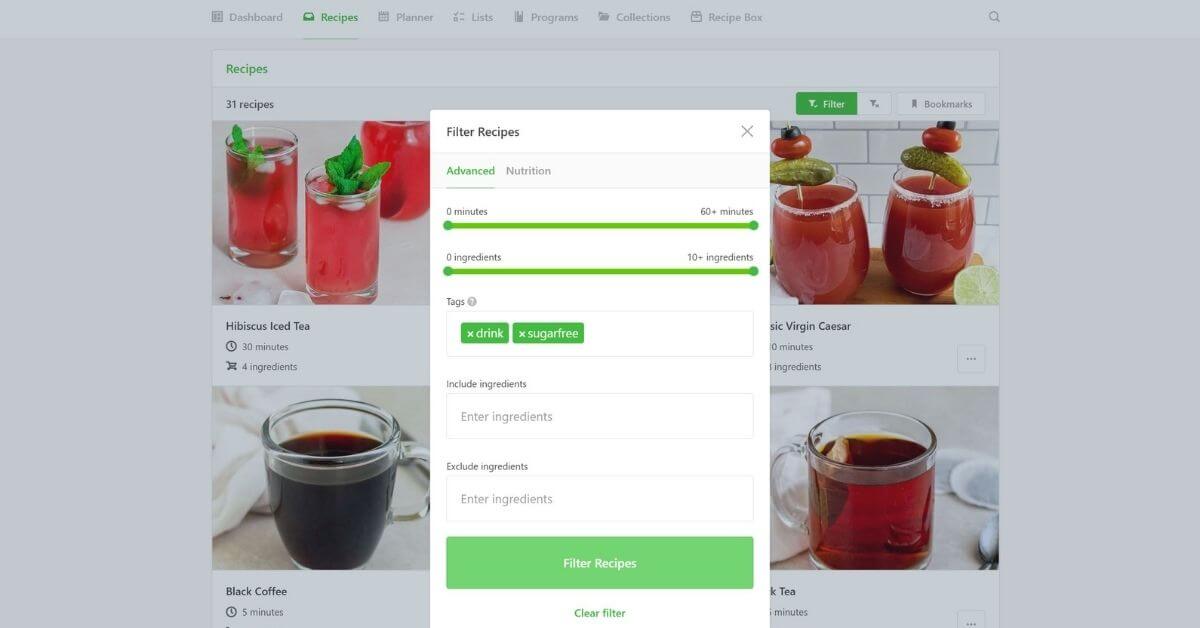
Tip: Use the drink and sugar-free filter within That Clean Life to easily find fun recipes to stay hydrated.
5. Maintain Oral Health
Diabetes increases the risk of gum disease, and periodontal diseases may also initiate insulin resistance and worsen glycemic control. People with diabetes who smoke are at an even higher risk to develop thrush and periodontal disease. Smoking also seems to impair blood flow to the gums, which might affect wound healing in this tissue area.
Ask your clients about what they do to keep good oral health and hygiene. This can include brushing and flossing as the first line of defense against tooth and gum problems, as well as regular checkups and cleanings at the dentist. If your client smokes, help them find resources and support to quit smoking.
Tip: Check out our Low Glycemic Diet, which includes a meal plan, grocery list, recipes, prep guide, and supporting evidence.
In addition to providing your clients with a low glycemic nutrition plan, work with them on incorporating these strategies to further regulate their blood sugar levels. A holistic approach is likely to lead to better health in the long term.

