Although they’re not new, GLP-1 medications have exploded in the field of weight management recently. Most of us know at least one person using them to help their weight loss goals, many of whom may be your clients. As a nutrition practitioner, you may be wondering how to best help your clients taking GLP-1s optimize their wellness, especially when creating personalized nutrition plans.
Dietitians play an essential role in supporting clients using GLP-1s, helping them make necessary dietary adjustments to maximize the medication's effectiveness, promote satiety, and ensure balanced nutrient intake.
We sat down with That Clean Life member Prabhsimran Saini, RD, MHSc, CDE, who is an expert in diabetes nutrition and working with GLP-1 medications, to talk about how she approaches meal planning for these clients.

What are GLP-1 medications and how do they work?
GLP-1 medications, or glucagon-like peptide-1 receptor agonists, are a class of drugs primarily used to manage type 2 diabetes and, more recently, obesity. They work by mimicking the action of the GLP-1 hormone, which is naturally produced in the gut when we eat.
Saini notes that GLP-1 medications have several mechanisms of action, some of which are still being unraveled in terms of how they help with weight management.
GLP-1 (the hormone) helps regulate blood sugar levels – and presumably supports weight management — in three ways:
- Stimulating insulin secretion to help move glucose from the bloodstream and into the cells to be used for energy
- Preventing the liver from releasing glucagon, a hormone that increases blood sugar
- Slowing gastric emptying and promoting feelings of fullness, helping to prevent mindless eating or overeating
GLP-1s can also reduce appetite and support weight loss goals by targeting the brain’s satiety and reward centers.
Some of the most common GLP-1 medications many people are being prescribed for weight loss include:
- Semaglutide: Wegovy® (FDA-approved for weight loss), Ozempic® (prescribed off-label)
- Liraglutide: Saxenda® (FDA-approved for weight loss), Victoza® (prescribed off-label)
- Tirzepatide: Mounjaro® (prescribed off-label), which is a dual GLP and GIP agonist, meaning it mimics the action of both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP), a hormone produced in the gut also involved in regulating blood sugar
Interestingly, Saini says, GLP-1s also appear to have other health benefits researchers are still learning about. “Some GLP medications have been shown to have protective benefits, especially for individuals with type 2 diabetes, reducing the risk of cardiovascular events like heart attack and stroke.” She says newer research is also suggesting that they have positive and protective benefits on individuals in terms of dementia and Alzheimer's risk.
How GLP-1 medications impact appetite
One of the things that makes GLP-1 medications so effective in helping clients achieve their weight loss goals is how they impact appetite. There are several mechanisms by which this happens.
First, GLP-1s interact with specific receptors in the brain that are involved in regulating hunger and satiety cues. Because of how they mimic the GLP-1 hormone, GLP-1 medications activate GLP-1 receptors in the brain.
These medications also help slow down gastric emptying, keeping food in the stomach for longer and preventing dramatic spikes in blood sugar levels. Saini says, “That delay in digestion helps keep people full for longer, and [this] reduces their food intake and helps in that weight management approach. Now, when your stomach is full for a longer time, it's going to signal the brain, ‘Hey, I'm full; I don't need more food.’”
Finally, GLP-1 medications reduce the release of ghrelin, often called “the hunger hormone.” This helps curb the desire to eat and supports overall caloric reduction. Some research suggests that certain GLP-1s may even affect taste perception in a way that reduces appetite.
Why dietitians need to be involved
GLP-1 medications have thus far been a largely doctor- and pharma-centered industry. Saini says there are a lot of reasons for this. First, “It is a pharma-led industry, so when physicians are talking, it's just better marketing for them because, unfortunately, a doctor has more say than a dietitian does in this day and age regarding authority and medical care.”
She also says that when dietitians enter the picture, patients realize GLP-1s aren’t some “miracle drug” and that there are other essential aspects to optimizing health and weight management.
Saini underlines the importance of dietitians being more involved in the nutritional management of patients using GLP-1s, saying, “These [medications] are directly reducing appetite, and when we're reducing appetite, we're reducing caloric intake. That means we now have a smaller window of opportunity to maximize or optimize nutritional status.”
As adding GLP-1 medications to someone’s routine reduces their overall desire to eat, it’s critical to focus on nutrient-dense foods in the diet. Keeping nutrient-dense foods at the forefront helps clients obtain the essential nutrients they need while having a calorie deficit.
What does eating look like when taking GLP-1 medications?
Fiber.
Much like you would encourage any client wanting to improve their health, those using GLP-1s should be counseled to prioritize high-fiber foods like fruits, veggies, whole grains, nuts, seeds, and legumes to support healthy blood sugar levels and satiety. However, Saini notes that fiber intake should be individualized based on a client’s tendency to get diarrhea or other digestive issues.
Lean protein.
Including plenty of lean proteins like fish, poultry, legumes, and soy products is important for promoting fullness and preserving lean muscle mass while losing fat. “You're technically supposed to be on [GLP-1s] once you start forever. And if that is happening, you're at higher risk for lean muscle mass loss. And that's why I think preserving muscle mass is one of the most important priorities regarding dietary recommendations,” says Saini.

Healthy fats.
Healthy fats from foods like avocados, olive oil, nuts, and seeds should precede foods high in saturated and trans fats. Finally, clients on GLP-1 medication should minimize consumption of ultra-processed foods and beverages that are high-calorie and nutrient-poor, like things high in added sugar, as these work against the goals of using GLP-1s.
Nutrient density.
Saini recalls working with a client on Ozempic who ate mostly bagels and bags of chips. “Imagine you're eating that because you feel full. It's a very calorically dense food. You're already having delayed gastric emptying. These are foods really low in fiber and can increase chances of constipation or bowel obstruction later if we're not optimizing their diet. They can also increase the risk for malnutrition.”
Hydration.
Finally, hydration is key, especially when GLP-1s slow gastric emptying and have a tendency to cause constipation. “We want to make sure that the patient is having a balanced approach, and limit highly processed foods, sugary foods, refined carbs, and high-fat, greasy foods [that can worsen digestive symptoms],” Saini notes. When maintaining your client's fiber intake, you can find creative ways to also increase their fluids.

Micronutrients.
GLP-1 medications can be very effective for achieving weight loss goals when used as directed and with other evidence-based lifestyle habits. However, using them could potentially increase the risk of certain nutritional imbalances if dietary intake isn’t carefully managed with appetite reduction. “If individuals are not eating as much, and we're not improving their relationship with food, or we're not improving their food habits, there can be a higher risk for malnutrition,” Saini says.
Plus, because it’s not uncommon to experience more digestive-related side effects when using GLP-1s like Ozempic, nausea, vomiting, constipation, and/or diarrhea can further set someone up for nutrient imbalances.
She recommends practitioners pay extra attention to nutrients like iron, calcium, vitamin D, and the B vitamins. A multivitamin with minerals can be a great tool to help clients ensure they’re filling micronutrient gaps when their food intake is reduced.
Macronutrient breakdown for clients on GLP-1s.
In terms of macronutrient breakdowns, Saini makes the following recommendations based on what she has experienced in her practice:
- Protein: “0.8-1 grams per kilogram at least. I try to aim for 1.2-1.6 grams per kilogram of protein if they're very active, if we see that they are at higher risk for malnutrition, or if we just want to be more careful in preserving their lean muscle mass, especially if it's an elderly status.”
- Carbs: “I tend to go a little bit lower, in the 40-50% range, as that helps us be consistent with their goals of type 2 diabetes management and weight loss.”
- Fat: “[I keep] fat at around 25-35%, focusing on healthier fats because we need those healthy fats for the hormone production, satiety, and absorption of key micronutrients like vitamins A, D, E, and K.”

How to use That Clean Life to create a supportive diet when taking GLP-1 medications
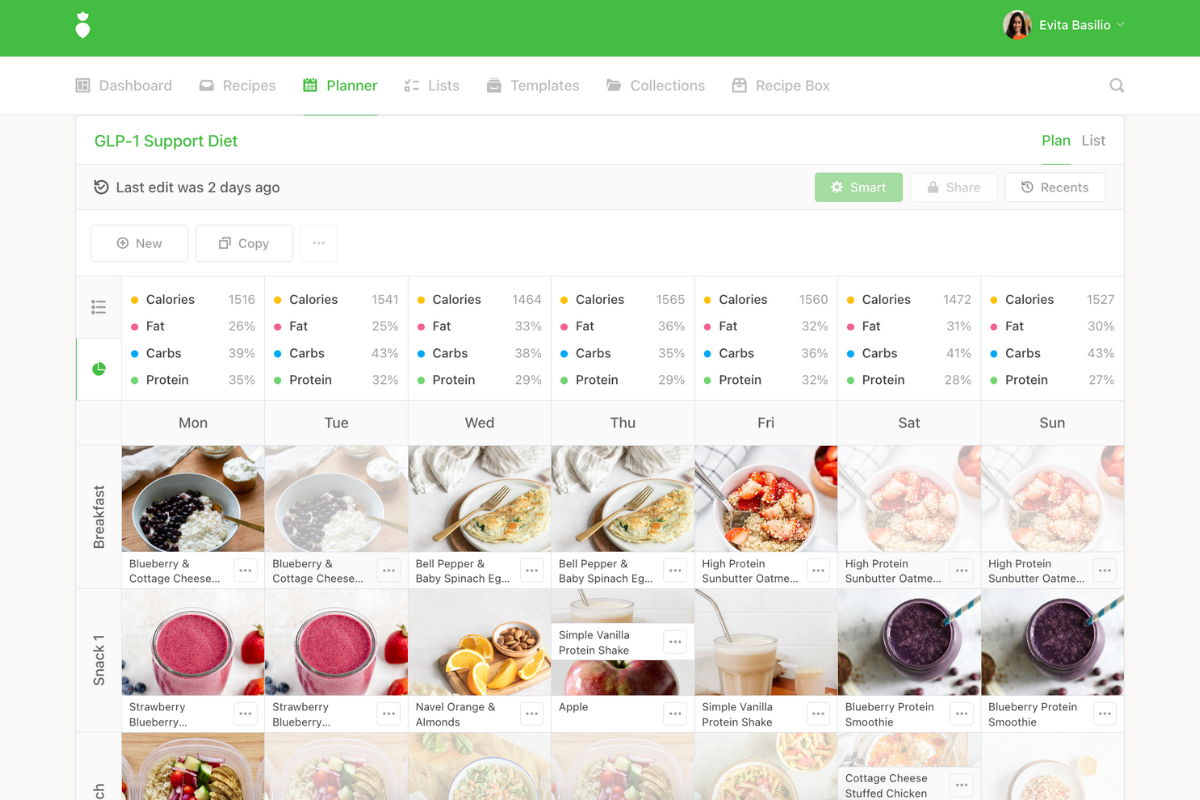
If you’re working with clients using GLP-1 medications, That Clean Life is here to support your needs and streamline your practice. We’ve recently designed and launched new templates for our practitioners specifically for this purpose.
Check out the GLP-1 Support Diet and Plant-Based GLP-1 Support Diet templates.
Our templates are made to save you time, are evidence-based, consistent in their professional quality, and allow for personalization to your client’s unique needs.
Dietitians and GLP-1s: Final thoughts
Dietitians are a cornerstone in clients' success in losing weight and improving their health, with or without GLP-1s. The latter, however, has a unique need for dietitians to step in and help patients on a more personal level, equipping them with a care plan that optimizes their nutrition and health outcomes alongside weight loss goals.
At the end of the day, Saini says, “We shouldn't demonize the medication. It’s a tool in our toolbox, and it does have a lot of positive benefits on overall health. So I think what we need to do is take our attention and our energy off of stopping people from going on it and instead help them navigate the drug. And that's where we, as dietitians, become more useful.”
Check out the new templates from That Clean Life to help you design eating plans for your clients using GLP-1 medications.

