The CDC estimates that about 23% of adults suffer from arthritis and the prevalence of this joint disease is only expected to increase. People with arthritis experience a decreased quality of life often due to physical limitations, pain, and mental health issues.
Nutrition is key in helping clients with arthritis and can reduce disease symptoms such as pain, joint stiffness, swelling, tenderness, and disability.
When it comes to developing a nutrition plan for a client with arthritis, there are many aspects to consider. In this article, we will cover the three key areas to focus on when nutrition planning for a client with arthritis including:
- Bone-building nutrients.
- Anti-inflammatory foods.
- Addressing deficiencies.
Meal Planning for Clients with Arthritis
Giving your clients with arthritis nutrition guidance is one thing, but helping them actually follow the guidance is another challenge altogether. A meal plan is a great way to take the nutrition guidance you are giving and turn it into an evidence-based roadmap that your client can easily follow and thus be more successful.
There are different types of arthritis, each of which requires a unique approach. But in general, when creating a meal plan for a client with arthritis, these are the key things you should focus on.
1. Bone Building Nutrients: Calcium, Magnesium, Potassium, Vitamin C & Vitamin D
Research shows that people with rheumatoid arthritis can be at higher risk for osteoporosis due to bone erosion. This makes it crucial for clients to meet their daily calcium, magnesium, and potassium needs. These minerals play a structural role in bone maintenance and modulate potential bone-damaging inflammation.
Focus on incorporating calcium-rich ingredients into your arthritis nutrition plans including fortified milk beverages, Greek or coconut yogurt, and fish with bones. Magnesium can be incorporated from food sources like cocoa powder, pumpkin seeds, and chia seeds. Potassium is found in many fruits and vegetables.

Vitamin C is an essential element of bone collagen and helps to control inflammation and pain. Adding more vitamin C-rich foods like kiwi, bell peppers and strawberries can help decrease symptoms of arthritis.
Tip: Use That Clean Life's filters to easily find recipes high in calcium, magnesium, potassium, and vitamin C.
Vitamin D helps to increase the absorption of calcium to build stronger bones. Vitamin D deficiency is prevalent worldwide and has been linked to several chronic inflammatory diseases, including rheumatoid arthritis. Obtaining sufficient vitamin D from natural (non-fortified) food sources alone is difficult so experts recommend that adults take a vitamin D supplement year-round.
2. Anti-Inflammatory Foods: Omega-3 Fatty Acids, Fiber & Antioxidants
Research suggests that omega-3 fatty acids can help clients with inflammatory arthritis by alleviating joint stiffness and pain. They have been found to suppress inflammation and modulate the immune response. Incorporate omega-3 fats into your arthritis nutrition plans by including foods such as salmon, plant-based oils, nuts, and seeds.

An imbalance in gut bacteria is often found in clients with arthritis as well as in those at-risk to develop arthritis. Fiber can restore microbial homeostasis and lowers C-reactive protein (CRP), a substance in the blood that indicates inflammation and is also associated with risk of cardiovascular disease events and diabetes. Current dietary guidelines recommend that adults consume over 25 grams of fiber per day, including both soluble and insoluble fiber. Help your clients increase their fiber intake by including whole grains, legumes, fruits, and vegetables in their meal plan.
Antioxidants such as vitamin E, carotenoids, and selenium may help protect joints by removing some of the compounds in the body that cause inflammation. These nutrients can be found in plant-based oils, nuts, and seeds, and brightly colored fruits and vegetables such as oranges, bell peppers, pumpkins, tangerines, and papayas.
Cruciferous vegetables like broccoli, kale, and cabbage contain sulforaphane which may help prevent or slow the progression of osteoarthritis. The compound is found to exert an anti-arthritic effect by regulating B-cell differentiation.
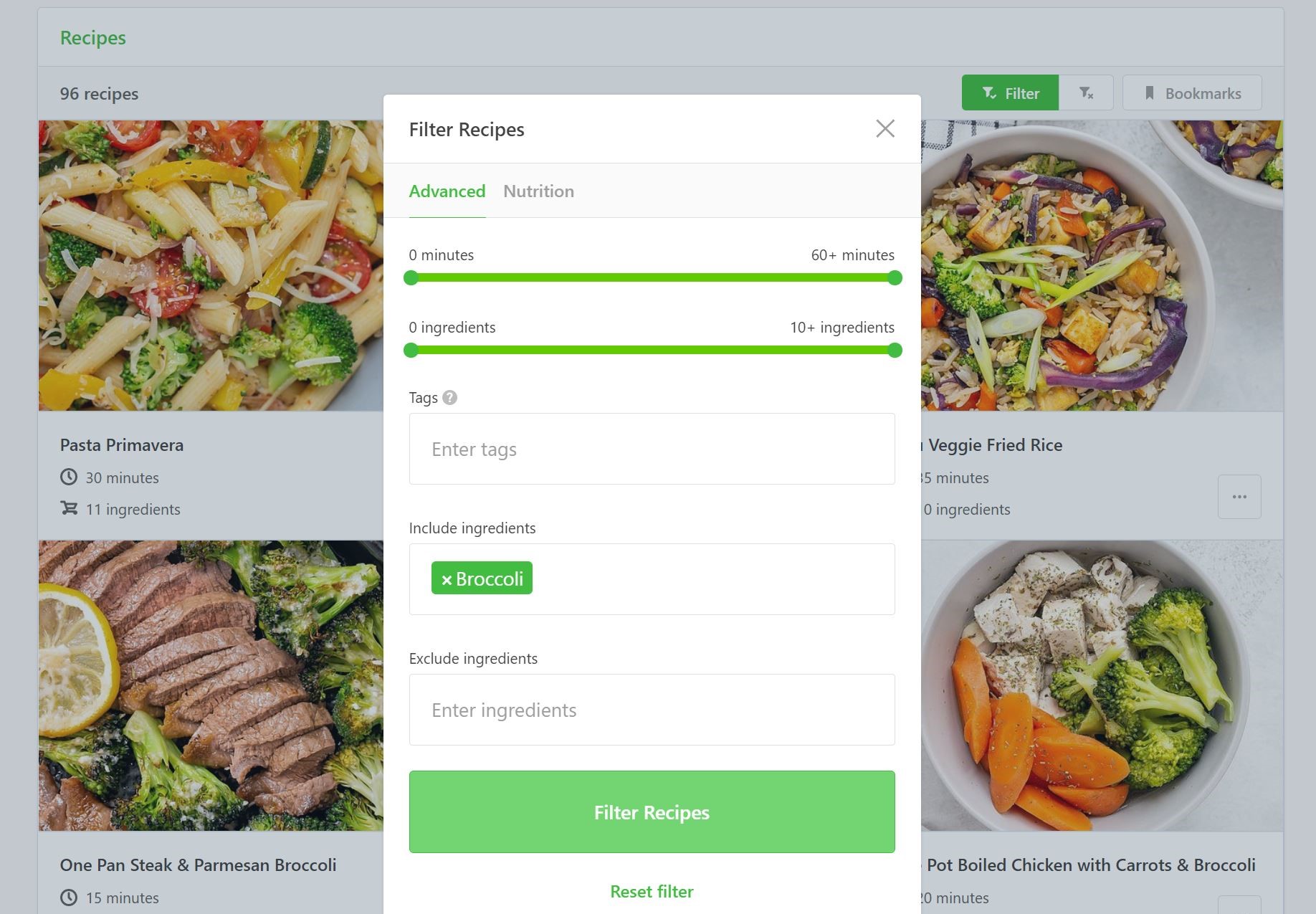
Tip: Find recipes that use cruciferous vegetables on That Clean Life by using the 'Include ingredients' filter.
Anthocyanins found in red and purple fruits like cherries, strawberries, raspberries, blueberries, and blackberries have antioxidant and anti-inflammatory properties. This helps reduce the frequency of gout attacks and may help ease the swelling associated with gout, a type of arthritis.

Polyphenols can act as antioxidants by neutralizing harmful free radicals that would otherwise damage your client’s cells. Polyphenols are found in dark chocolate, berries, apples, grapes, oats, and turmeric.
3. Addressing Deficiencies: Iron & Folate
Long-term use of certain arthritis medications can lead to nutrient deficiencies. During your meal planning assessment, ask your clients about any medications and supplements they may be taking to identify possible food and drug interactions and potential deficiencies. Nutrient deficiencies should be confirmed with laboratory testing.
Many people with arthritis have anemia, which means they do not have enough hemoglobin or red blood cells. This may result from inflammation and certain medications. To help maintain the health of red blood cells and prevent anemia, it is important to get enough iron.
There are two types of iron found in foods: heme iron (from red meat and other animal products) and non-heme iron (from spinach, legumes, and dried fruit). For better absorption of non-heme iron, encourage clients to pair it with vitamin C-rich foods like citrus, tomatoes, or peppers at mealtime.

Long-term use of arthritis medications may lead to nutrient deficiencies. For example, patients receiving methotrexate often have folic acid deficiency. Spinach, liver, asparagus, and brussels sprouts are among the foods with the highest folate levels. Getting enough folic acid can also reduce common methotrexate side effects such as nausea, vomiting, and liver toxicity.
Tip: Use That Clean Life’s filters to find recipes that meet your client’s daily iron and folate requirements.
Nutrition and meal planning is one piece of helping your clients with arthritis. Medications and exercise are also important. Encourage your clients to stay active as this can decrease pain by keeping joints and cartilage healthy.
Key Takeaways
- Nutrition is key in helping clients with arthritis and can reduce disease symptoms such as pain, joint stiffness, swelling, tenderness, and disability.
- When developing nutrition plans for clients focus on bone building nutrients like calcium, magnesium, potassium, vitamin C and vitamin D.
- Incorporate omega-3 fatty acids, fiber and antioxidants to help reduce inflammation.
- Address common deficiencies in arthritis like iron and folate by incorporating foods like red meat, liver, spinach, asparagus, legumes, and dried fruit.
- For better absorption of non-heme iron, encourage clients to pair it with vitamin C-rich foods like citrus, tomatoes, or peppers at mealtime.
Tip: Check out That Clean Life's Arthritis Program and Plant-Based Arthritis Program which have been designed to include these important nutrients. Both come with a meal plan, grocery list, recipes, prep guide, supporting evidence, and include the key considerations mentioned.