Inflammatory bowel disease (IBD) is a term for two conditions, Crohn’s disease and ulcerative colitis. Both are characterized by chronic inflammation of the gastrointestinal (GI) tract and treatment options include:
- Pharmacotherapy
- Surgical removal of diseased areas of the GI tract
- Elimination diets to improve symptom management and induce or maintain remission, such as the Specific Carbohydrate Diet
What is The Specific Carbohydrate Diet?
The Specific Carbohydrate Diet (SCD) allows carbohydrate foods consisting of monosaccharides only and excludes disaccharides and most polysaccharides, such as linear or branch-chained multiple sugars or starches. This diet is based on the theory that disaccharides and polysaccharides pass undigested into the colon, which results in bacterial and yeast overgrowth, overproduction of mucus, and this may cause intestinal injury.
The SCD was introduced in the 1920s by gastroenterologist, Sidney Haas. It was then expanded and popularized in the 1980s with Elaine Gottschall’s definitive SCD guide in the book, Breaking the Vicious Cycle: Intestinal Health Through Diet.
Who is The Specific Carbohydrate Diet For?
There is an increasing body of evidence that shows the SCD is a viable option for maintaining remission in adult and pediatric Crohn’s disease and ulcerative colitis. The SCD may help improve symptoms, decrease inflammation and may lead to increased biodiversity of the microbiome. Some research found a change in the microbiome of patients with IBD who followed the SCD, including reversal of some of the dysbiosis reported in patients with IBD.
Foods to Eat & Avoid
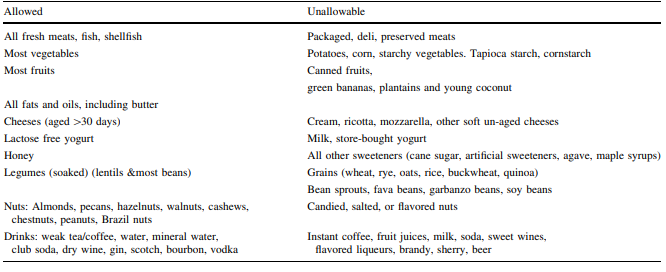
The SCD allows almost all fruits and vegetables containing more amylose (a linear-chain polysaccharide) than amylopectin (a branch-chained polysaccharide), nuts, nut-derived flours, dry-curd cottage cheese, meats, eggs, butter, and oils.
It excludes sucrose, maltose, isomaltose, lactose, grain-derived flours, and all true and pseudograins, potatoes, okra, corn, fluid milk, soy, cheeses containing high amounts of lactose, as well as most food additives and preservatives. The SCD isn't necessarily a low-carbohydrate diet, but it's extremely specific about the types of carbohydrates that are permitted.
The diet is supplemented by homemade yogurt fermented for 24 hours to free it of lactose, a disaccharide not allowed in the SCD. Recommended cultures include Lactobacillus bulgaricus, Lactobacillus acidophilus, and Streptococcus thermophilus. You can find a homemade coconut yogurt recipe here.

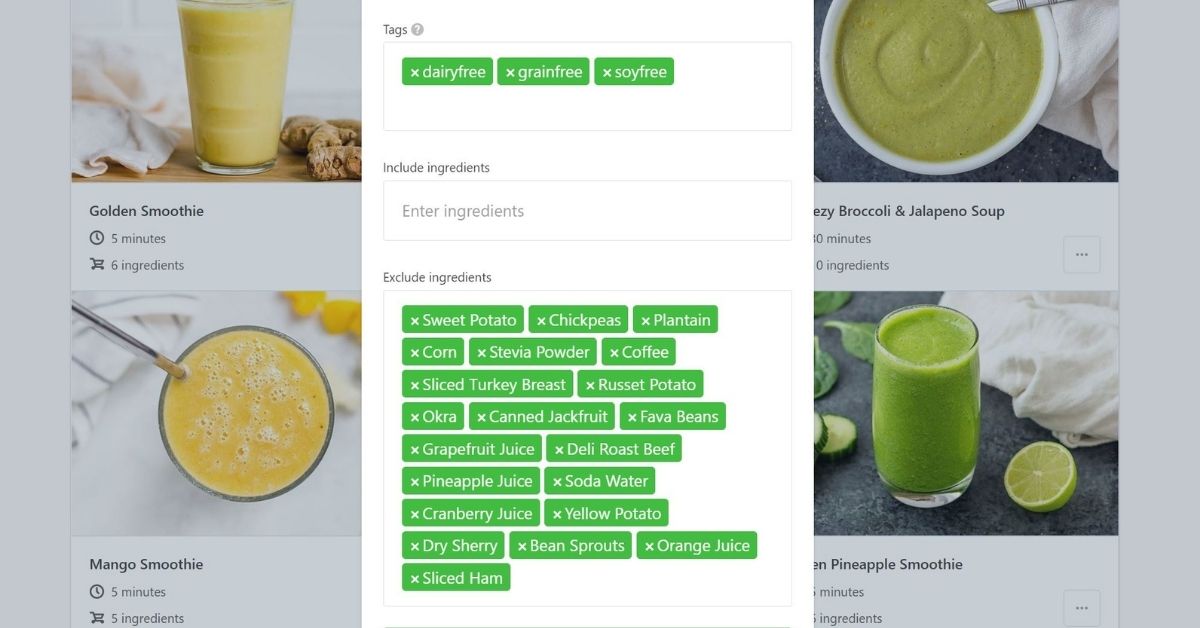
Tip: Use That Clean Life's Specific Carbohydrate filter to find SCD recipes and our Specific Carbohydrate Diet Programs for full done-for-you meal plans with grocery lists, recipes, prep guides, and supporting evidence.
The Specific Carbohydrate Diet Steps
The SCD can be modified based on the client's unique response to foods. Prior to starting a client on the SCD, the nutrition professional should educate both the client and their family on the diet and the work that it entails. The diet is implemented in three steps:
1. Diet Introduction
Once the client begins the SCD, they should follow up with their healthcare provider in one to two weeks. These first visits with the healthcare professional are to ensure that individuals are maintaining their weight or at least have minimal weight loss, their symptoms are under control, their laboratory studies are within an acceptable range, and it is an opportunity for clients to ask about specifics in regard to the diet.
2. Maintenance
If the client goes into remission, then they can proceed to the diet foundation and maintenance step with reduced follow-up. The efficacy of the SCD should be judged at the earliest in one month. There should be an assessment of symptoms using appropriate symptom scores and also markers of inflammation including CRP, fecal calprotectin, and possibly colonoscopy if clinically appropriate. If there are no improvements in symptoms and/or inflammation, it may be reasonable to discontinue the SCD and consider other therapeutic options available.
3. Food Reintroduction
This step involves reintroducing foods that were previously eliminated. Data suggests that an attempt to liberalize the diet should occur preferably after the disease is well controlled and is in the inactive phase. This step does not necessarily need to happen and has no set time frame. Clients may or may not want to reintroduce foods. This step can be important for clients who struggle with maintaining the strict SCD. The most important aspect of this step is to reintroduce foods slowly and one at a time, closely monitor symptoms and laboratory studies, as well as fecal calprotectin levels to ensure that inflammation is not rebounding.

The diet should be closely monitored by a nutrition professional to assess for potential deficiencies. Nutritional deficiencies that can possibly occur with the SCD including folate, thiamine, vitamin B6, D, C, A, calcium and potassium deficiencies.
As with all of these recommendations, adjusting for each individual’s unique needs is important and often necessary. Following the SCD with guidance from a nutrition professional could optimally nourish a patient with IBD.
IBD is a complex medical condition and the SCD intervention may improve symptoms in some people, however there is no guarantee that it will work for everyone. Clients require proper meal planning and preparation to make it easier to follow the diet. Other dietary strategies proposed for managing symptoms of IBD include the Low Fodmap Diet, Anti-Inflammatory Diet for IBD (IBD-AID), gluten-free, lactose-free, Mediterranean or Paleo diets.