Reflux is also called Gastroesophageal Reflux Disease or GERD. It happens when contents from the stomach back up, or reflux, into the lower esophagus - the tube connecting the mouth and stomach. Normally when a person eats, a muscle in the lower esophagus closes after food goes into the stomach. The muscle is called a sphincter. It closes to stop the food from going back up into the esophagus. Reflux happens when the lower esophageal muscle does not close properly.
GERD symptoms can include heartburn, tightness in the chest, unpleasant taste in the mouth, dry cough that does not go away, wheezing, voice roughness, and a feeling that one needs to clear their throat often.
Meal Planning for Clients with Gastroesophageal Reflux Disease
Diet and lifestyle changes can play a major role in controlling acid reflux symptoms and is the first line of therapy used for clients with GERD.
At That Clean Life, we offer a Gastroesophageal Reflux Disease (GERD) Program and Plant-Based Gastroesophageal Reflux Disease (GERD) Program which focus on eliminating common trigger foods for reflux, avoiding added sugars, and emphasizes foods that help reduce symptoms such as fiber, healthy fats, and lean protein.
Our GERD Programs include a 7-day meal plan, itemized grocery list, recipes, prep guide, and supporting evidence. They can be customized based on your client’s energy needs and preferences.
Foods to Eliminate
Trigger Foods
Our programs exclude certain foods that can reduce the lower esophageal sphincter tone and motility, cause mucosal irritation, or increase gastric juice secretion. These trigger foods include spicy and fatty foods, high-fat dairy products, certain spices, citrus fruits and juices, acidic foods and beverages, coffee and black tea, chocolate, mint products, onions, garlic, and tomato-based products.
Food triggers can vary for each client and should be adjusted for each individual’s unique needs.
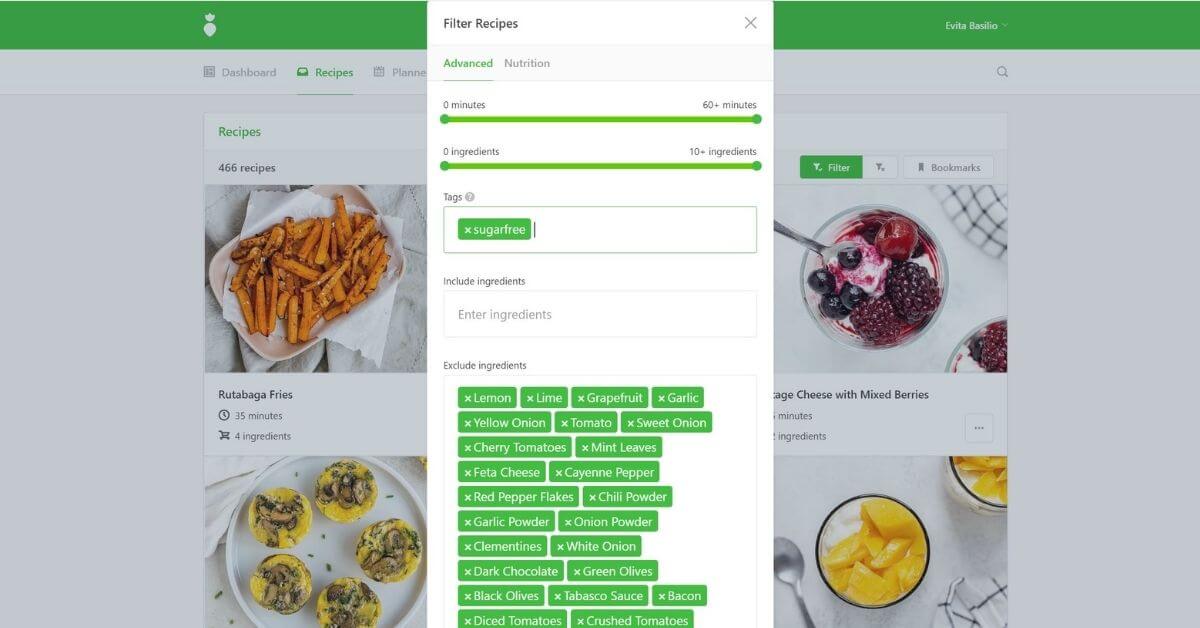
Tip: Use That Clean Life's filters to easily find recipes that meet your client's requirements. For example, you can filter for recipes that exclude known food triggers for your client.
No Added Sugars
Simple sugars raise blood sugar levels and produce an osmotic effect in the gastrointestinal tract. Sweets with peppermint, spearmint, and chocolate can often cause pain. To prevent this effect and minimize reflux symptoms, our GERD programs are sugar-free, focus on whole foods, and avoid artificial sweeteners as these can negatively alter gut microbiota.

Foods to Add
Fiber
Regular and adequate intake of fiber is associated with decreased heartburn symptoms. Our GERD programs are rich in vegetables, fruits, and whole grains to provide a daily fiber goal of up to 45 grams. Soluble fiber found in foods like oats, bananas, dates, lentils, and sweet potatoes are added to the programs as this type of fiber is found to decrease symptoms and esophageal pressure. Certain fruits and vegetables are eliminated in the program such as citrus fruit and juice, tomato, onion and garlic, green pepper, radish, avocado, and olives due to their effect on reflux symptoms.
Healthy Fats & Plant-Based or Lean Protein
High fat diets, especially those which include increased amounts of saturated fat from fried or greasy foods and creamy sauces can worsen reflux symptoms. Fat takes longer to leave the stomach which can cause further symptoms. Animal protein sources from lean meats, fish and poultry, eggs, cottage cheese, and low-fat cheese are better options. Fried and highly spiced meats, as well as processed deli meats should be avoided. Our programs use plant-based or lean protein options, healthy omega-3 fats from walnuts, and monounsaturated fatty acids from seeds, avocado, pecans, almond butter, and olive oil.

Lifestyle
Lifestyle and behavior changes have been shown to reduce the symptoms of reflux and should be combined with your client's GERD meal plan. Some recommended lifestyle modifications include:
- Eat several smaller meals or snacks a day rather than three large meals. Having smaller amounts of food in the stomach allows more time for digestion and prevents stomach acid from backing up into the throat.
- Eat and drink slowly and chew foods well. Avoid chewing gum, drinking pop or fizzy beverages, and using straws as swallowing more air can worsen symptoms.
- Avoid eating or drinking two hours before lying down to avoid backflow of stomach contents. Try raising the head of your bed to prevent backflow.
- When eating, sit up straight with your shoulders back.
- Avoid wearing tight clothing across the stomach and chest.
- Avoid smoking as nicotine relaxes the lower esophageal sphincter.
- Aim to achieve a healthy body weight as added weight increases intragastric pressure.
GERD is often treatable through a combination of lifestyle changes, nutrition, and medication as needed. But persistent symptoms of reflux need a thorough evaluation by a gastroenterologist who can find the underlying cause and discuss available treatment options.

